“Is there any evidence UVc light disinfection routines can actually be attributed to patient decrease in HAIs or Hospital-acquired Multiple-drug-resistant organisms (MDROs)?”
CLICK FOR FULL STUDY
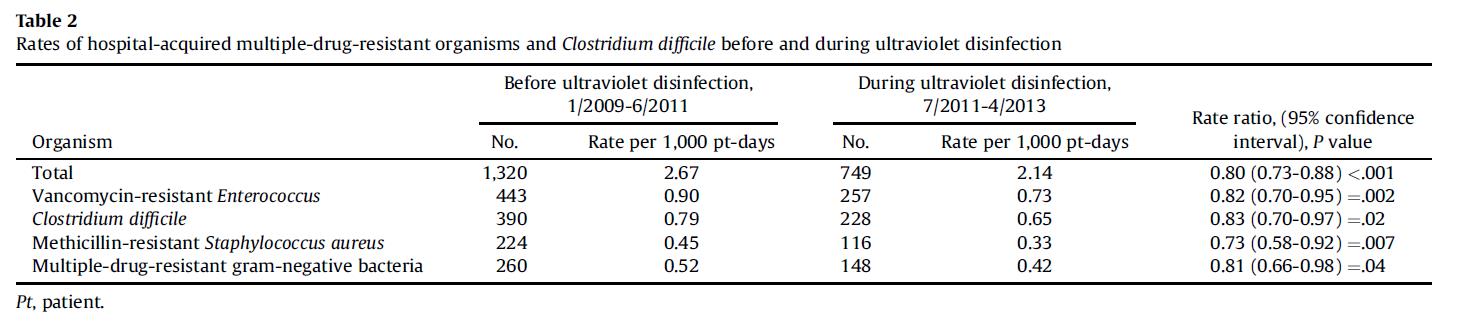
In this study (click to gain access to full study above) Westchester Medical Centre in Valhalla, NY, performed 11,000 UVc secondary disinfections over 22 months (2011 – 2013) resulting in a significant 20% incidence decrease in overall hospital-acquired infections, or Hospital-Acquired MDROs, including CD, MRSA and VRE, compared to the baseline of 30 previous months prior (2009 – 2011). This decrease was sustained during the UVc disinfection period reported in this study. The occurrence reduction could have been significantly larger, to an estimated 25% or more of HAIs (Hospital acquired MDROs and CD) if UVc disinfection was:
- Performed in all contact-precautions rooms at discharge (24% were missed due to multiple reasons listed in the study). And,
- Was performed with an autonomous UVc device like the UVD UVc robot. - As we note and explain in: “A) Items to note in this study” below.
I think you will find the attached study and its conclusions provide sufficient evidence that UVc light disinfection does significantly reduce the occurrences of HAIs or Hospital-Acquired MDROs and makes a good case to start regular UVc secondary disinfections at your earliest opportunity.
We would suggest that these results can be improved upon with the use of an autonomous UVD UVc disinfection robot due to:
- Greatly reduced disinfections times,
- Ease of use, and efficiencies gained,
- And eliminating “shadowing” and “involuntary omissions” to provide more certainty in disinfection.
- Key items to note in this study:
- The study used UVc disinfection after primary cleaning of contact precautions rooms.
- This study was conducted prior to the introduction of autonomous UVD UVc devices and used two static or pushcart UVc units. – this resulted in much longer disinfection times, and, with only three positions used, this study may not have maximised certainty in disinfection as shadowing would have occurred.
- The use of static or pushcart UVc units resulted in much longer disinfection periods per disinfection – 51 minutes per room / area – and so a reduced efficiency. (Please see breakdown provided below Note 1)
- The study deployed for longer, 6 min disinfections per “position”, to A) try and have the light reach further distances and B) as the pulse xenon bulbs, using UVa, UVb and UVc, is a much broader use of the light spectrum, other than just UVc, it requires a longer exposure for the UVc portion of the “pulsed light” to be effective. Our mercury UVc bulbs concentrate on just the 254 nm wavelength required for maximum germicidal properties to destroy the RNA and DNA of pathogens.
- Finally, the study deployed the units for only 76% of occurrences, missing 24% of rooms needing a secondary disinfection.
- During the study they did stop disinfecting the OR’s due to the amount of time a cleaning person was diverted to the secondary or terminal clean. Again, we note our autonomous UVD robot would disinfect the average OR in a maximum 15-minute period where a static or push-cart unit would require many repositioning’s, and thus “warm-ups”, taking at least 75 minutes or longer for the average OR. The UVD autonomous robot provides a substantial savings of time therefore efficiencies and costs providing an ROI that pays for the robots.
- It was noted in the study that Mercury bulbs (like the UVD Robot lamp) produced a 99% reduction of CD whereas xenon pulse bulbs resulted in a 53% reduction of CD.
- Other relevant information:
- The hospital UV disinfections were performed between July 1, 2011 – April 20, 2013. They were performed in the following areas:
- Rooms of contact-precautions-discharge patients - 3,833 uses (34% of total uses)
- Patient rooms upon staff request - 3,695 uses (32%)
- Routine operating room and burn unit - 1,938 uses (17%)
- Bathroom disinfection of an occupied room - 1,938 uses (17%)
- During the study period, the average discharge time increased by 51 minutes due to use of static or pushcart UVc disinfection device. Those 51 minutes can be significantly reduced with newer autonomous technology (UVD Robots) and efficient usage routines coordinated by Environmental Services.
- In total, UVc machines in this hospital were used only 30% of the available time due mostly to personnel resources unavailability, likely caused by the length of time, 51 minutes, to disinfect a single occurrence. An autonomous UVD UVc robot would greatly reduce this time to an estimated 11 minutes. Continuous improvement through the use of autonomous UVc devices is expected and should deliver even higher reduction of HAIs beyond the 20-25% range presented above.
- Several implementation considerations were defined and monitored to optimize the use of UVc disinfection. These included incorporating a quick digital request/need for UVc disinfection in the Environmental Services process and communications routine. Supervisors were trained and personnel from manual disinfection were assigned to operate the UVc disinfection devices.
- In summary, the implementation of UVc disinfection to reduce HAIs can now increase its effectiveness through automation capabilities and joint team planning between Environmental Services, Infection and Prevention Control and the different relevant hospital areas. Regency Robotics and UVD Robots is committed to support our partners during implementation and roll-out to reach highly satisfactory results.
- The VRE acquisition rates experienced during this UVc disinfection period were the lowest incidence rates of VRE at the Westchester Hospital for the past 10 years.
“Although there were many other simultaneous infection control interventions occurring at our hospital during the period from 2009 until 2013 that could have contributed to the reduction in VRE acquisition, the rates experienced during UVD are the lowest incidence rates of VRE at our institution for the past 10 years and were sustained for 22 months.”
Note 1 Disinfection times breakdown from the study: (our estimate) Three positions @ 6 minutes each = 18 minutes, plus 3 separate “bulbs warm up periods” (due to pushcart stop and start) @ 3 minutes each = 9 minutes, for 27 minutes total, plus a min of 5 minutes per position “pushcart moving and set up time” = 15 minutes for a total of 52 minutes per disinfection. Again, Regency feels only two positions in the patient room is not enough to eliminate shadowing to achieve the certainty in disinfection which suggests to us, with an autonomous unit, they could have achieved much better than a 20% reduction in HAIs over the 22-month period. The autonomous UVD robot would have completed these disinfections in an estimated 11 minutes including one “bulbs warm up” period of just 3 minutes.
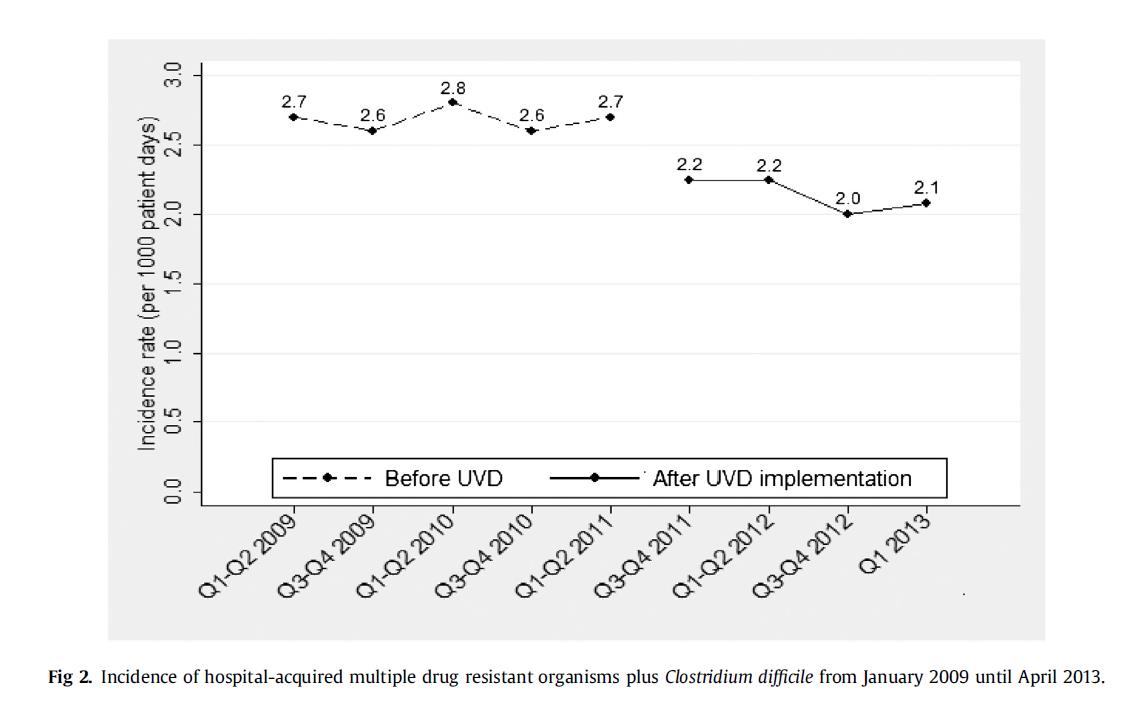
CHART: a significant 20% incidence decrease in overall hospital-acquired infections, or Hospital-Acquired MDROs over 22 months.
This table shows the incidence rates of VRE, CD, MRSA and MDR gram-negative organisms were significantly lower during the UVc period.